Written By: Anju Dheer, PT, DPT, OCS, MTC
 As a new graduate, the diagnosis of spondylolisthesis in my patients filled me with anxiety. It wasn’t extensively covered in school, with professors often dismissing it as an uncommon diagnosis—just something to be aware of. Fast forward a few years, and I found myself treating numerous patients with spondylolisthesis diagnoses or findings in their X-rays or MRIs. This realization prompted me to delve deeper into the subject.
As a new graduate, the diagnosis of spondylolisthesis in my patients filled me with anxiety. It wasn’t extensively covered in school, with professors often dismissing it as an uncommon diagnosis—just something to be aware of. Fast forward a few years, and I found myself treating numerous patients with spondylolisthesis diagnoses or findings in their X-rays or MRIs. This realization prompted me to delve deeper into the subject.
Understanding that a clinician’s lack of confidence can adversely affect patient outcomes, I dedicated myself to researching this condition. As my knowledge grew, so did my treatment effectiveness, resulting in improved patient outcomes. In light of this, I decided to create a webinar to support other clinicians who might be in a similar situation. If you’re one of those clinicians, be sure to sign up for my upcoming webinar on Spondylolisthesis Treatment (November 9th).
Understanding Spondylolisthesis
Having a solid pathoanatomical foundation combined with strong clinical decision-making skills is crucial in managing this common condition. Often, spondylolisthesis is a radiological diagnosis characterized by the slippage of one vertebra over another. Interestingly, patients may be asymptomatic or experience pain from a different source.
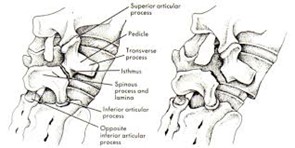
 The incidence of low back pain is on the rise, yet despite increasing healthcare spending on its management, outcomes have worsened. One significant reason for this discrepancy is the non-specific nature of low back pain. While spondylolisthesis can be a source of specific low back pain, low-grade degenerative spondylolisthesis typically is not. In contrast, isthmic spondylolisthesis—associated with a fracture of the pars interarticularis—often serves as a specific source of low back pain. This condition is identifiable by the classic “scotty dog with a collar” appearance on oblique lumbar X-rays. Learn how the management strategies differ between isthmic and degenerative spondylolisthesis in my upcoming course.
The incidence of low back pain is on the rise, yet despite increasing healthcare spending on its management, outcomes have worsened. One significant reason for this discrepancy is the non-specific nature of low back pain. While spondylolisthesis can be a source of specific low back pain, low-grade degenerative spondylolisthesis typically is not. In contrast, isthmic spondylolisthesis—associated with a fracture of the pars interarticularis—often serves as a specific source of low back pain. This condition is identifiable by the classic “scotty dog with a collar” appearance on oblique lumbar X-rays. Learn how the management strategies differ between isthmic and degenerative spondylolisthesis in my upcoming course.
Management Strategies
We will explore the following strategies:
- Conservative rehabilitation and post-operative management
- A comprehensive approach that can be applied to various lower back conditions
- Progression of exercises from:
- Local activation
- Static stabilization
- Dynamic stabilization
- Return to sports/function
I hope you’ll join me in exploring this important topic further. Register today and let’s enhance our understanding and improve outcomes for our patients!
CLICK HERE to view Anju Dheer‘s Instructor Page.
References
- Bydon, M., Alvi, M. A., & Goyal, A. (2019). Degenerative Lumbar Spondylolisthesis: Definition, Natural History, Conservative Management, and Surgical Treatment. Neurosurg Clin N Am, 30(3), 299-304. doi: 10.1016/j.nec.2019.02.003. PMID: 31078230.
- Gould, H. P., Winkelman, R. D., Tanenbaum, J. E., et al. (2020). Epidemiology, Treatment, and Performance-Based Outcomes in American Professional Baseball Players With Symptomatic Spondylolysis and Isthmic Spondylolisthesis. The American Journal of Sports Medicine, 48(11), 2765-2773. doi: 10.1177/0363546520945727.
About Summit Professional Education
Summit equips Physical Therapists, Occupational Therapists and SLPs with better continuing education courses that provide CEUs while impacting patient outcomes. Find high-quality on-demand CE along with the largest offering of live options — including live webinars, live streams, and in-person courses. Want to deep dive on a topic? Summit offers hundreds of 6-hour courses for the most in-depth learning!




